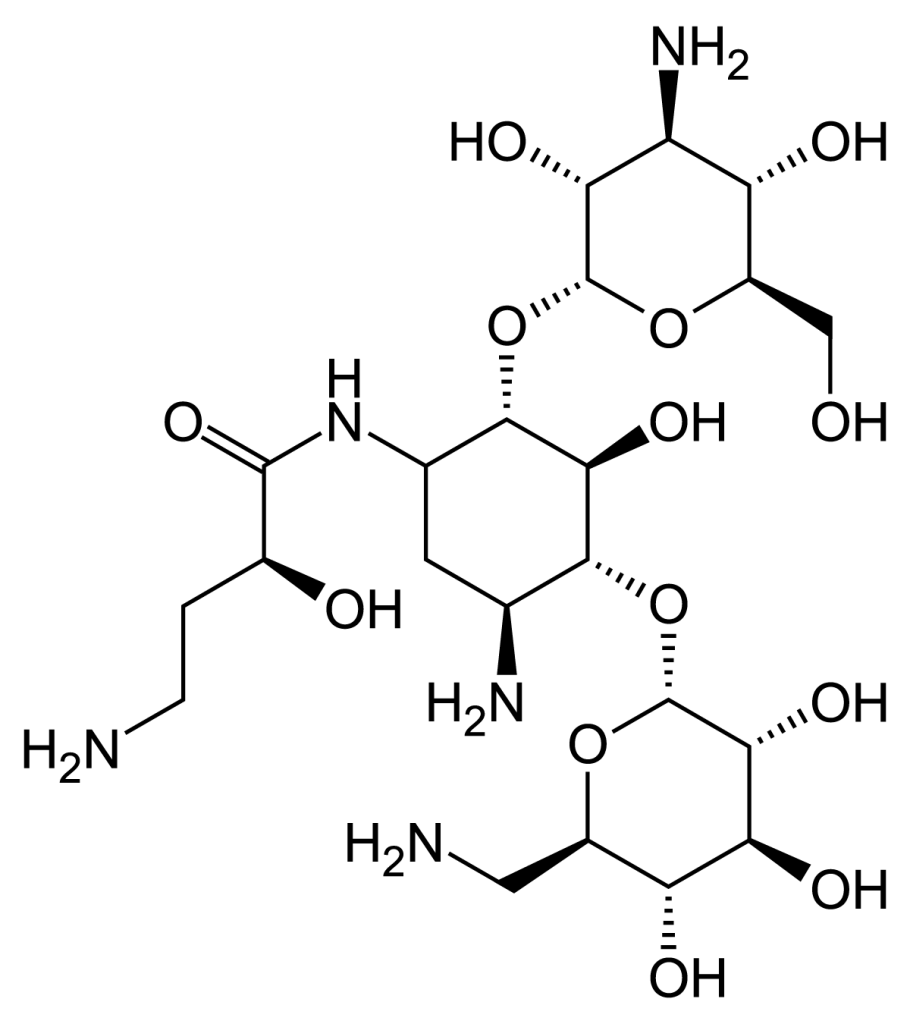
Amikacin is an antibiotic belonging to the aminoglycoside group, known for its efficacy in treating serious infections caused by Gram-negative bacteria. This drug is used in settings where pathogens are often resistant to other antibiotics, such as gentamicin and beta-lactams, and is a crucial resource in the fight against antibiotic resistance. However, as with any antibiotic treatment, its use requires care to balance efficacy and potential side effects.
Based on a number of scientific studies including the “Rapporto AR-ISS 2022” and the article bearing the signatures of P. G. Gooding, E. Berman, A. Z. Lane and K. Agre’s “A review of results of clinical trials with amikacin” -two of the most comprehensive and authoritative studies relatively to the topic-we observe how Amikacin represents today the drug with the best efficacy in terms of cure rate with the lowest level of antibiotic resistance when comperated with others commonly used against bacterial infections.
Mechanism of Action
Amikacin acts by inhibiting bacterial protein synthesis. It interferes with peptide formation, leading to the production of aberrant proteins that impair vital bacterial functions. This mechanism causes damage to the plasma membrane, resulting in loss of potassium and eventually cellular breakdown. This effect is particularly potent against Gram-negative bacteria such as Pseudomonas aeruginosa (which we will discuss in the next section), Serratia, Proteus, Klebsiella, Enterobacter, and Escherichia coli, especially when these prove resistant to other aminoglycosides.
Clinical Efficacy of Amikacin
A study of 1,098 patients in 10 countries showed that Amikacin resulted in cure in 81% of the 697 patients eligible for drug efficacy evaluation. This outcome was observed through clinical remission and eradication of infectious pathogens. Genitourinary infections responded best to treatment, with a 90% efficacy rate, followed by septic infections (85%) and skin, soft tissue or bone infections (70%). Amikacin was also effective against gentamicin-resistant pathogens, with an 88% success rate in infections sustained by these bacteria.
The standard dose used was 7.5 mg/kg, administered intramuscularly every 12 hours. In patients with renal impairment, the dosage was adjusted to prevent complications related to drug accumulation.
Amikacin and Antibiotic-Resistance.
One of the most critical aspects of the use of Amikacin is its role in combating antibiotic resistance. This antibiotic is effective in situations where many other drugs fail, especially against resistant Gram-negative bacteria, such as strains of Pseudomonas and Klebsiella.
Resistance rates for Pseudomonas aeruginosa remain critical for some classes of antibiotics. In 2022, for example, 24.1 percent of P. aeruginosa isolates were resistant to piperacillin-tazobactam, 19.0 percent to ceftazidime, and 16.4 percent to carbapenems such as imipenem and meropenem. Despite this, resistance to aminoglycosides, including Amikacin, remained at the lowest level (4.0%), making it still an effective option in many cases. However, prudent use of this drug is essential to prevent Amikacin from losing its efficacy as well.
Pseudomonas aeruginosa and Antibiotic Resistance.
Gram-negative bacteria: antibiotic resistance profile for Pseudomonas aeruginosa, Italy 2022
| Class of antibiotics | Antibiotic | Isolated (n) | R (%) | 95% CI R (%) |
| Penicillins | Piperacillin-Tazobactam | 5.893 | 24,1 | 23,0 – 25,2 |
| Cephalosporins III/IV generation | Ceftazidime | 5.903 | 19,0 | 18,0 – 20,0 |
| Cefepime | 5.775 | 17,5 | 16,5 – 18,5 | |
| Ceftazidime/Avibactam | 3.726 | 6,0 | 5,2 – 6,8 | |
| Ceftolozane/Tazobactam | 3.322 | 5,5 | 4,7 – 6,3 | |
| Carbapenemes | Imipenem | 5.019 | 17,7 | 16,6 – 18,8 |
| Meropenem | 5.816 | 9,5 | 8,7 – 10,3 | |
| Aminoglycosides | Amikacin | 5.855 | 2,7 | 2,3 – 3,1 |
| Gentamicin | 818 | 12,6 | 10,4 – 15,1 | |
| Tobramycin | 3.248 | 6,9 | 6,0 – 7,8 | |
| Fluoroquinolones | Ciprofloxacin | 5.943 | 16,2 | 15,3 – 17,2 |
| Levofloxacin | 1.874 | 21,1 | 19,3 – 23,1 |
R=resistance; CI=confidence interval
From 2015 to 2022, decreasing trends were observed in the percentage of Pseudomonas aeruginosa isolates resistant to the major classes of antibiotics used to treat these invasive infections. In particular, since 2017, there has been a steady decline in resistance to aminoglycosides, such as Amikacin, and fluoroquinolones. However, for other drug classes, such as ceftazidime and piperacillin-tazobactam, resistance has remained relatively stable. As for carbapenems, after an increase in resistance in the previous two years, a slight decrease was noted in 2022.
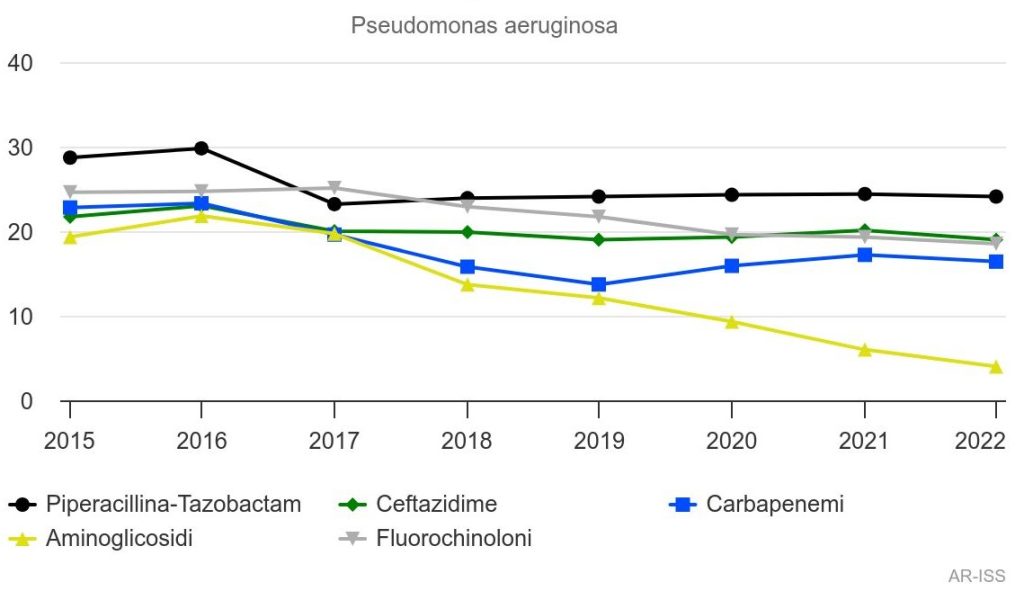
Percentage of resistance of Pseudomonas aeruginosa to piperacillin-tazobactam, ceftazidime, carbapenems, aminoglycosides and fluotoquinolones (Italy 2015-2022)
As highlighted in the graph above, in 2022 the highest resistance rates for Pseudomonas aeruginosa were observed for piperacillin-tazobactam (24.1%), followed by ceftazidime (19, 0%), fluoroquinolones such as ciprofloxacin and levofloxacin (18.5%), carbapenems such as imipenem and meropenem (16.4%), and aminoglycosides with a low 4.0% for amikacin and gentamicin. This finding confirms the continued efficacy of Amikacin against resistant bacterial strains, highlighting that its ability to combat serious infections, especially those caused by multi-resistant pathogens such as Pseudomonas aeruginosa, is still very relevant.
Sitography:
Pseudomonas aeruginosa – Sorveglianza dell’Antibiotico-Resistenza – AR-ISS
A review of results of clinical trials with amikacin – PubMed (nih.gov)